Clay County Medical Center Improves Care Transitions Processes

Care transitions, particularly from an inpatient setting to home, can be a challenging time for patients who may be dealing with a medical crisis, a new medical condition, or change in care plan. Poor transitions of care can lead to a variety of negative outcomes, including medication discrepancies, adverse clinical events, poor patient experience of care, and frequently avoidable hospitalizations. Improving care transitions has been an important strategy for reducing the costs associated with hospitalization and readmissions1 and proves to be an important opportunity for addressing social determinants of health2. Transitional Care Management (TCM) serves to manage this hand-off period offering an excellent opportunity for primary care providers to oversee and coordinate support for a patient's medical conditions, mental health or behavioral health needs, social services, and other barriers to optimal patient outcomes.
2024 KHC Leadership in Quality Awards Winners Announced

2024 Leadership in Quality Awards submissions were featured in a Virtual Storyboard Showcase during the Summit on Quality Awards on August 8th in Wichita. Winners in each category were announced during the Leadership in Quality Awards Luncheon following the Virtual Storyboard Showcase.
2024 KHC Leadership in Quality Awards Submissions

Submissions have been received for the 2024 KHC Leadership in Quality Awards. Winners will be announced during the Leadership in Quality Awards Luncheon at the KHC Summit on Quality, August 8th in Wichita, KS.
Rural Kansas Community Collaborates in Response to Local Opioid Crisis

More than one million people have died since 1999 from a drug overdose.1 In 2021, 106,699 drug overdose deaths occurred in the United States. The age-adjusted rate of overdose deaths increased by 14% from 2020 (28.3 per 100,000) to 2021 (32.4 per 100,000).
Rooks County Health Center Selected as a 2023 Health Quality Innovator of the Year

Award recognizes Rooks County Health Center’s dedication to improving health in Plainville and Rooks County.
Plainville, KS — Rooks County Health Center (RCH) has been recognized as a Health Quality Innovator for 2023. The Health Quality Innovator Awards is the annual awards program created by Health Quality Innovators (HQI) that recognizes and celebrates organizations that are using successful, evidence-based approaches to improve health care quality and outcomes.
Success Story - Southwest Medical Center Tackles Sepsis Bundle Compliance

More than 1.7 million people in the U.S. are diagnosed with sepsis each year1. 350,000 adults die from sepsis every year in the U.S. which represents more deaths than opioid overdoses, breast cancer, and prostate cancer combined1. Southwest Medical Center (SWMC), an acute care hospital located in Liberal, KS, joined Compass HQIC in September 2020. As they assessed their priorities for the Compass HQIC Workplan, they identified Sepsis Bundle Compliance as a priority for improvement through their work with Compass HQIC.
Health Partnership Clinic Closes Gaps in Colorectal Cancer Screening

Health Partnership Clinic, an FQHC with four clinic sites in Olathe, Ottawa, Paola, and Shawnee Mission, serves a population of more than 15,000 patients each year, the majority of which are underserved and uninsured. Serving a patient population facing additional social drivers of health and barriers to care creates challenges in managing and screening for chronic disease. Through their work with the Kansas Healthcare Collaborative and KDHE in the CDC's Colorectal Cancer Control program, Health Partnership Clinic has developed innovative strategies to increase access to care and increase screening rates in their underserved patient population.
F.W. Huston Medical Center Focuses on the Individual Patient to Reduce Readmissions

F.W. Huston is a 25 bed Critical Access Hospital in Winchester, in Northeast Kansas and is a member hospital in the Compass HQIC Network. When Nancy Martin, a former employee of F.W. Huston Medical Center, returned to the hospital as Director of Nursing in August of 2022, she noticed some trends in care transitions that were attributed to an increase in readmissions. Patients were returning to F.W. Huston or other hospitals after hospital discharge in cases where it seemed preventable. Nancy and the F.W. Huston Team would embark on a quality improvement project that after nearly one year has made strides in process improvements, yet admittedly is still under construction.
Genesis Family Health Sews the Seeds of Health with CHWs

At the start of the new year in 2023 Genesis Family Health looked at the issues facing their community and wanted to find ways to use community outreach to engage their expectant mothers in health education. Their Care Team came up with the idea to gather maternity patients together to create baby gifts or to make items needed for their new babies and wanted to use those gatherings to share health education with expectant mothers.
Nemaha Valley Community Hospital Addresses Health Equity in Local Amish Community

In April 2017, church elders from the nearby Amish community met with two physicians and a social worker from Nemaha Valley Community Hospital (NVCH) to discuss concerns about recent poor birth outcomes in both mothers and babies in the local Amish community. A meeting between physicians and church elders to solve health care issues is not the norm in healthcare, but in this case, was the most logical and culturally appropriate means to address an issue, which was vital to both the Amish community and the hospital.
CHCSEK Healthy Heart Ambassador Sucess Story

Rooks County Health Center partners with community stakeholders to address workforce challenges

In March 2022, the American Hospital Association urged Congress to address workforce issues affecting health care facilities1. AHA called those workforce issues “a national emergency that demands immediate attention from all levels of government and workable solutions." According to the Kansas Hospital Association’s 2022 Workforce Report2 vacancy and turnover rates in 2021 for licensed practical nurses and staff nurses were higher than in all previous years dating back to 2013. Statewide, overall employee turnover rate for surveyed health care positions averaged 19%, with the highest turnover rates for housekeepers (33%), food service workers/dietary aids (31%) and Certified Nursing Assistants (29%).
Spotlight: Holton Community Hospital achieves 46% reduction in readmissions amid COVID-19
Hospitalizations account for nearly one-third of the total $2 trillion spent on health care in the United States, according to the Institute for Healthcare Improvement. Though most hospitalizations are necessary, too often patients are re-admitted soon after their initial hospital stay. Such readmissions are both costly and often avoidable.
Holton Community Hospital (HCH) in northeast Kansas achieved a 46% improvement in their Unplanned All Cause 30-Day Readmissions Rate between September 2020 and February 28, 2022. Through their work with HQIC and the KHC, they implemented a unique Readmission Risk Assessment and developed a proactive approach to care coordination, which resulted in the dramatic improvement of the hospital’s readmission rate.
Kansas Hospital Spotlight: Suits to Scrubs Initiative
 Participants in the Suits Initiative in the Siena Pediatric Ward at St. Catherine's Hospital in Garden City, Kansas. From left to right: Michelle Beatriz, MA; Veronica Medrano, RN; Judy Morales, MA; Jessica Hestikind, RN, Samantha Walck, RN; and Stephanie Waggoner, Regional Director of Operations for Centura Health Physician Group.
Participants in the Suits Initiative in the Siena Pediatric Ward at St. Catherine's Hospital in Garden City, Kansas. From left to right: Michelle Beatriz, MA; Veronica Medrano, RN; Judy Morales, MA; Jessica Hestikind, RN, Samantha Walck, RN; and Stephanie Waggoner, Regional Director of Operations for Centura Health Physician Group.
This summer, an innovative idea was spurred via St. Catherine Hospital’s regular employee engagement survey. Haley Evans — the hospital’s Director of Quality and Patient Safety Officer — said the idea stemmed from how the pandemic has affected care delivery, in ways both big and small. While the bigger issues may sometimes be easier to address as they get the most attention, the smaller issues can compound and chip away at staff morale the longer they go unaddressed. She said the employee’s idea was to help leadership see firsthand the changing circumstances in which they are providing care.
Regional hospital in Southwest Kansas takes proactive steps to prevent patient falls
 Pictured are Southwest Medical Center’s (SWMC) staff who have been instrumental in assisting with its Focus on Falls initiative. Front row, left to right: Avery Ysac, CNA; Erin Guitron, CNA; Reyna Tarango, W/C; Courtney Chim, RN; Marian Eruagbere, RN; Jentry Strothman, LPN; and Beji Saji, RN. Back row left to right: Michael McCallion, LPN; William Salvador, LPN; Nichole Eatmon, CNA; Jaime Torres, CNA; Gissell Uribe, RN; and Mirella Buchman, RN, Nurse Manager.
Pictured are Southwest Medical Center’s (SWMC) staff who have been instrumental in assisting with its Focus on Falls initiative. Front row, left to right: Avery Ysac, CNA; Erin Guitron, CNA; Reyna Tarango, W/C; Courtney Chim, RN; Marian Eruagbere, RN; Jentry Strothman, LPN; and Beji Saji, RN. Back row left to right: Michael McCallion, LPN; William Salvador, LPN; Nichole Eatmon, CNA; Jaime Torres, CNA; Gissell Uribe, RN; and Mirella Buchman, RN, Nurse Manager.
Southwest Medical Center (SWMC) is a not-for-profit acute care hospital with 89 beds in Liberal, Kansas, also serving patients from nearby Colorado, Oklahoma, Texas, and New Mexico.
As part of their participation in the Compass HQIC program in partnership with KHC, SWMC identified falls prevention as one of its top patient safety goals. This is, in part, because the hospital saw a spike in patient falls during 2020 as compared to 2019. SWMC is now in their first five months of planning, educating staff, and taking action on interventions. They named the initiative “Focus on Falls.”
Central Kansas community collaborates to address health needs amid COVID-19
 Team members of the community collaboration group in Ellsworth County, central Kansas.
Team members of the community collaboration group in Ellsworth County, central Kansas.
Among the focus areas for hospitals participating in the Compass Network is Community Collaboration and Integration. While the COVID-19 public health emergency has made working closely with others more challenging, community members in the central Kansas county of Ellsworth (pop. 6,231) saw it as an opportunity to forge partnerships to address health needs.
Creating a sustainable culture of safety: Hiawatha's hand hygiene improvements amid COVID-19

A small, community hospital in northeast Kansas came together with a splash of fun and accountability to create a sustainable culture of safety, especially when it comes to hand hygiene.
As the COVID-19 pandemic made its way across the nation earlier this year, the Hiawatha Community Hospital was wrapping up its participation in a statewide Hand Hygiene Collaborative facilitated by the Kansas Healthcare Collaborative. The nine-month initiative concluded in March, 2020, with more than 60 Kansas hospitals participating.
Staff from Kansas providers and KHC trained for Diabetes Prevention Program
Twelve team members from clinics and hospitals in Kansas—along with two KHC Quality Improvement Advisors—recently completed training to be certified Lifestyle Coaches under the National Diabetes Prevention Program (DPP).
The training was sponsored by the Kansas Department of Health & Environment and provided online by the Association of Diabetes Care & Education Specialists (ADCES).
A third of American adults—or 88 million people—have prediabetes. People with prediabetes are at higher risk of heart attack, stroke, and type 2 diabetes.
DPP programs are among those approved by CMS to help patients diagnosed with prediabetes work to prevent or delay the development of type 2 diabetes. Certified Lifestyle Coaches meet regularly with patients over the course of a year to lose at least 5% of their body weight through healthier eating and increased physical activity.
Hess Clinic: Using telemedicine for Chronic Care Management
 Team members at Hess Clinic in Hays are, front row from left: Gail Brack, LPN/CPC Office Manager; Samantha Harms, APRN; Katrina Hess, MD, clinic owner; Rhonda Kinderknect, LPN. On the back row from left: Shaundell Van Pelt, Administrative Assistant-Occupational Medicine; Kristin Mauch, CMA; Monica Gabel, AEMT/PHCT; Jennifer Goodale, RN. Not pictured: Cyndy Dreiling, Operations Manager.
Team members at Hess Clinic in Hays are, front row from left: Gail Brack, LPN/CPC Office Manager; Samantha Harms, APRN; Katrina Hess, MD, clinic owner; Rhonda Kinderknect, LPN. On the back row from left: Shaundell Van Pelt, Administrative Assistant-Occupational Medicine; Kristin Mauch, CMA; Monica Gabel, AEMT/PHCT; Jennifer Goodale, RN. Not pictured: Cyndy Dreiling, Operations Manager.
In early February, Hess Clinic began what would prove to be a prescient change in how they deliver health care. The clinic in Hays began seeing many patients via telemedicine—particularly those managing chronic conditions—nearly two months before Kansas declared its first stay-at-home order due to COVID-19.
Coffeyville Regional: Improving early recognition and treatment of sepsis
 Team members at Coffeyville Regional Medical Center.
Team members at Coffeyville Regional Medical Center.
Quality Improvement Goal: By January 1, 2020, the hospital aimed to improve to 100% adherence to all three-hour sepsis resuscitation treatment bundle guidelines.
Following a Joint Commission survey in December 2018, the team at Coffeyville Regional Medical Center (CRMC) realized they had taken an eye off the ball when it came to sepsis. They identified a gap in early identification of Systemic Inflammatory Response Syndrome (SIRS) criteria and organ dysfunction, as well as implementing appropriate CMS sepsis core measure interventions—specifically nurse-driven interventions.
Labette Health slashed readmissions by 43% since 2012 — here's how
 Some of the more than 700 team members at Labette Health.
Some of the more than 700 team members at Labette Health.
Quality improvement goal: Our goal was to reduce avoidable readmissions to as near to zero as possible.
We started in partnership with the Kansas Healthcare Collaborative in 2012 through the Hospital Engagement Network (HEN) 1.0, HEN 2.0, and the current Hospital Improvement Innovation Network (HIIN). Since then, we have grown in how we approach and monitor performance improvement projects. Early on, this institution felt that readmissions reduction was a quality department-driven objective — but over the course of this and other projects, we have seen a culture change in institution. Directors and front-line staff see the quality department as a tool and as support for accomplishing ambitious goals.
Dramatically reducing patient falls at Osborne County Memorial Hospital
 Osborne County Memorial Hospital team members (from left) include Cindy Hyde, Risk Manager; Kristen Hadley, Quality Improvement Coordinator; Lori Rothenberger, RN and Assistant Director of Nursing; and Monica Mullender, RN and Director of Nursing.
Osborne County Memorial Hospital team members (from left) include Cindy Hyde, Risk Manager; Kristen Hadley, Quality Improvement Coordinator; Lori Rothenberger, RN and Assistant Director of Nursing; and Monica Mullender, RN and Director of Nursing.
Quality Improvement Goal: Reduce patient falls with injury by 30% or more from 2018 to 2019.
The quality improvement team at Osborne County Memorial Hospital (OCMH) is led by Quality Improvement Coordinator Kristen Hadley. By participating in the statewide Hospital Improvement Innovation Network (HIIN) led by the Kansas Healthcare Collaborative (KHC), Hadley and her team have access to comparative data reports that help inform and guide the hospital’s quality improvement efforts.
“Our data reports indicated that we were coming in higher than the state average for falls,” Hadley said. “Leadership was on board from the beginning when we made a commitment and priority to preventing falls with injury.”
Newman Regional Health: Improving transitions of care, reducing readmissions
 Newman Regional Health team members (L to R) Cathy Pimple, Chief Quality and Compliance Officer; Nina Topper, Clinical Analyst; Dr. Alana Longwell, Hospitalist and Inpatient Rehabilitation Medical Director; and Aubrey Arnold, Care Manager.
Newman Regional Health team members (L to R) Cathy Pimple, Chief Quality and Compliance Officer; Nina Topper, Clinical Analyst; Dr. Alana Longwell, Hospitalist and Inpatient Rehabilitation Medical Director; and Aubrey Arnold, Care Manager.
Although readmission rates were already lower than their target, leadership at Newman Regional Health thought they could further reduce them.
Cathy Pimple is Chief Quality and Compliance Officer at the not-for-profit 25-bed critical access hospital in Emporia, owned by the citizens of Lyon County, Kansas. She said they recognized that those at highest risk for readmission in their community shared something in common.
“We recognized that our high-risk patients were individuals who had multiple chronic illnesses,” Pimple said. “So, in order to better address their needs, we developed an Advanced Illness Management (AIM) program, which was aimed at improving care transitions.”
Clinic presentations at the 2019 Innovator's Symposium
Five Kansas clinics were among the 40 Compass PTN participants that presented posters at the 2019 Innovator's Symposium in Atlanta. Download them below.
Enhancing Patient Engagement Through Trauma-Informed Quality Improvement
Caritas Clinics, Inc.
Kansas City
Contact: Jana Zaudke,
Lindsborg clinic sees quick success boosting Medicare Wellness Visits
 The Family Health Care Clinic team includes Karna Peterson (back row, fifth from right) and Julie Worcester (back row fourth from left), who led the push to increase Annual Wellness Visits among the clinic's Medicare patients.Annual Wellness Visits are a regular opportunity for Medicare patients and their physicians to give special attention to personalized prevention plan. Needed screenings are performed or scheduled, risk factors and treatment options are addressed, and diet, home safety, and available community resources can be discussed, among other things.
The Family Health Care Clinic team includes Karna Peterson (back row, fifth from right) and Julie Worcester (back row fourth from left), who led the push to increase Annual Wellness Visits among the clinic's Medicare patients.Annual Wellness Visits are a regular opportunity for Medicare patients and their physicians to give special attention to personalized prevention plan. Needed screenings are performed or scheduled, risk factors and treatment options are addressed, and diet, home safety, and available community resources can be discussed, among other things.
“It’s a time to give guidance or encouragement on important aspects of wellness that a provider and patient may not have time to discuss in a typical office visit,” said Karna Peterson, Clinic Manager at Family Health Care Clinic, which is part of Lindsborg Community Hospital.
Family Health Care Clinic (FHCC) was already exceeding the national average for percentage of patients getting Annual Wellness Visits (or AWVs), but they wanted to do better.
“We were seeing a lot of patients who weren’t taking advantage of all the screenings that they were eligible for, and the Annual Wellness Visit is a dedicated time to make sure that recommendations were done,” said Peterson. “I feel like it’s our duty as health care providers to help patients understand their benefits and the health care they have access to and can benefit from.”
Hiawatha clinic recognized as one of Kansas’ top five practices in improving health care quality, safety, and value
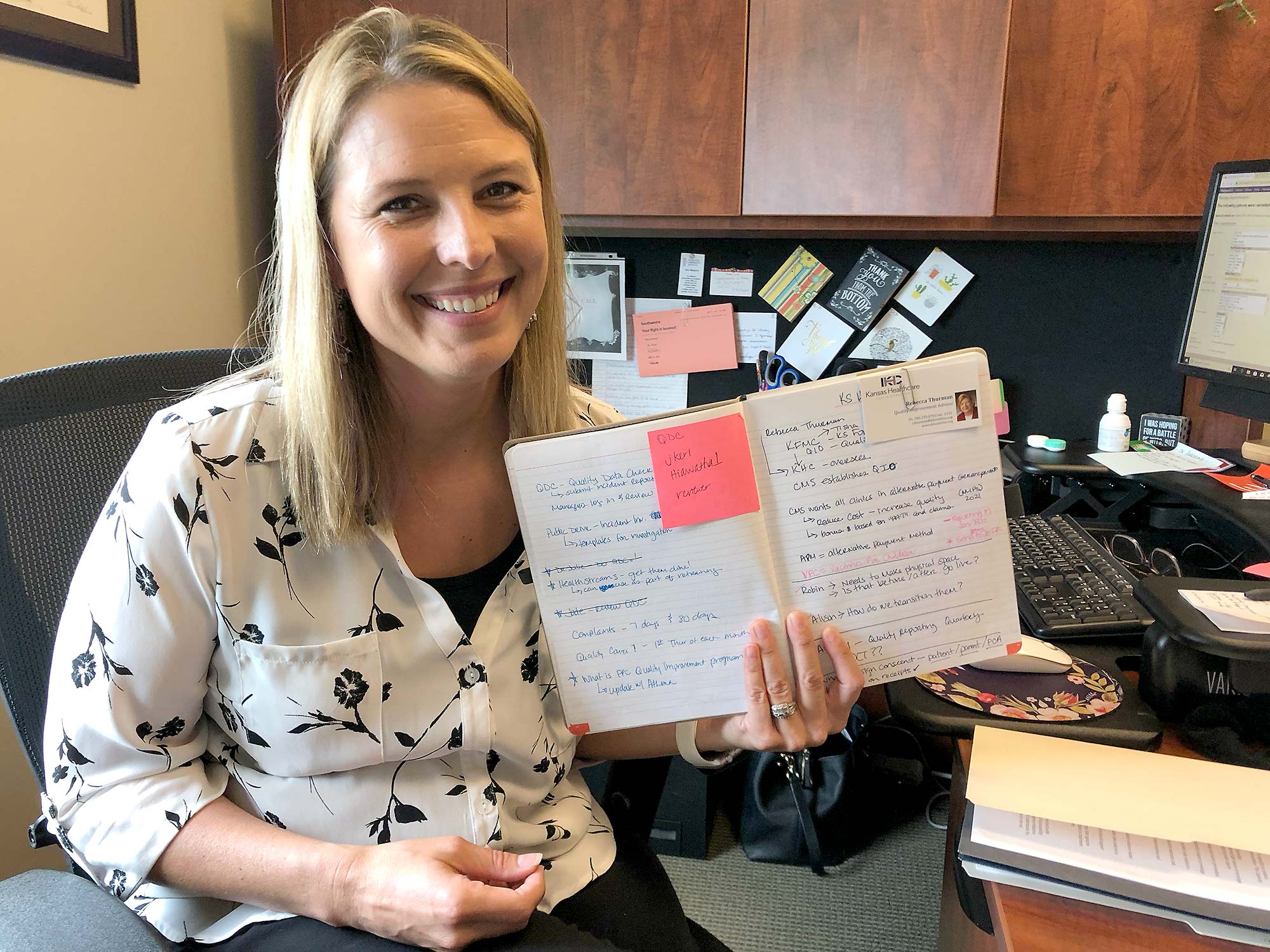 Jacquie Kerl, Hiawatha Family Practice Clinic manager, with the notebook she started during her first meeting with KHC.HIAWATHA—Jacquie Kerl still refers to the notebook she started during her very first meeting about quality improvement.
Jacquie Kerl, Hiawatha Family Practice Clinic manager, with the notebook she started during her first meeting with KHC.HIAWATHA—Jacquie Kerl still refers to the notebook she started during her very first meeting about quality improvement.
The clinic manager at Hiawatha Community Hospital keeps it with other reference material within reach of her keyboard. Clipped to the first page is the business card of Rebecca Thurman, her Quality Improvement Advisor from the Kansas Healthcare Collaborative (KHC).
“About a year ago, Rebecca showed up here on my second week on the job,” Kerl said. “She broke down everything, which was crucial. And since then every time I’ve had a question or concern, she’s been there. She’s always challenging me to take the next step—to make the next incremental improvement.”
Dr. Barrett recognized as one of Kansas’ top five practices in improving health care quality, safety, and value
 Mary and Dr. Bradley Barrett after recieving the Pinnacle Practice award in Atlanta earlier this summer.NEODESHA—Dr. Bradley Barrett is so focused on his patients that he hadn’t raised his fees in 10 years. His wife Mary, administrator of the clinic, knew they were low, but not by just how much.
Mary and Dr. Bradley Barrett after recieving the Pinnacle Practice award in Atlanta earlier this summer.NEODESHA—Dr. Bradley Barrett is so focused on his patients that he hadn’t raised his fees in 10 years. His wife Mary, administrator of the clinic, knew they were low, but not by just how much.
"We found out we were charging less than half of what Medicare allows in our area,” Mary Barrett said. “My husband has a feeling for those with less means. But we weren’t even charging insurance enough."
Mary said all that changed upon beginning work with the Kansas Healthcare Collaborative in 2017. Jill Daughhetee is the clinic’s KHC quality improvement advisor.
“Jill came in and helped us make our practice more financially sustainable immediately,” Mary said. “And at the same time, we’ve put practices into place that have helped us demonstrate the quality of care our patients receive.”
Women’s Health Center recognized as one of Kansas’ top five practices in improving health care quality, safety, and value
 Women's Health Center staff includes Jennifer Brady (right) and Tiffany Miller.CHANUTE—At the Women’s Health Center, every obstetrical patient is placed into a risk stratification group to help guide their care. A nurse screens all new patients at the first appointment, the physician reviews the screening and patient information, and the case receives a risk level.
Women's Health Center staff includes Jennifer Brady (right) and Tiffany Miller.CHANUTE—At the Women’s Health Center, every obstetrical patient is placed into a risk stratification group to help guide their care. A nurse screens all new patients at the first appointment, the physician reviews the screening and patient information, and the case receives a risk level.
“Risk stratification is a best practice, but there are significant challenges to putting it in place,” said Patty Thomsen, the clinic’s Quality Improvement Advisor from Kansas Healthcare Collaborative. “The most significant challenge is formalizing the process and ensuring that the policy and procedure flows for the clinical staff—which is part of the milestone for the Transforming Clinical Practice Initiative.”
“That's huge—early identification of at-risk pregnancies is absolutely one of the best things you can do to improve health outcomes now and well into the future. And of course, that usually translates into much few costly complications,” Thomsen said.
That’s where Women’s Health Center’s partnership with KHC is proven critical, said Clinic Manager Jennifer Brady.
Horizons Mental Health Center recognized as one of Kansas’ top five practices in improving health care quality, safety, and value
 Horizons Mental Health Center same-day access staff (Vikki Mader not pictured).
Horizons Mental Health Center same-day access staff (Vikki Mader not pictured).
HUTCHINSON—Staff at Horizons Mental Health Center thought they could improve access to care at their clinic, but they were shocked by just how much.
Horizons recently gathered feedback as part of the clinic’s patient and family engagement efforts and through meetings with community partners, said Vikki Mader, Health Information Management Director and Risk Manager at Horizons.
“One of the major complaints was that it took too long to get in to be seen for an initial visit,” Mader said. “Often the next day is just too long for someone struggling with a mental health issue." At that point, they were only able to schedule about 29 percent of initial visits on the same day.
So, in November, Horizons fundamentally changed their workflow.
NW Family Physicians recognized as one of Kansas’ top five practices in improving health care quality, safety, and value
 Northwest Family Physicians staff members, including clinic administrator Heather Steinert (third from left).WICHITA—Patient-centered communication helps improve health outcomes. At Northwest Family Physicians, patient-centered communication has led to nearly all of their diabetic patients bringing their condition under control, said clinic administrator Heather Steinert.
Northwest Family Physicians staff members, including clinic administrator Heather Steinert (third from left).WICHITA—Patient-centered communication helps improve health outcomes. At Northwest Family Physicians, patient-centered communication has led to nearly all of their diabetic patients bringing their condition under control, said clinic administrator Heather Steinert.
"Now we have a very small percentage of diabetics who are over 9 (not under control). I can think of only three patients currently—and that's fantastic," Steinert said, noting the clinic has more than 2,000 diabetic patients.
Exemplary Practice Story: Sunflower Ob-Gyn, Winfield
Sunflower Ob-Gyn—a clinic in Winfield and member of the Kansas Practice Transformation Network—began a program aimed at improving patient outcomes in hypertension, diabetes, and depression through weight loss. They called it "KDM Intense." Over 12 weeks, patients worked with a nutritionist, a trainer, a pharmacist, and staff at Sunflower to improve their diet, activity level, and blood pressure. The early results in the program have been impressive—including dramatic reductions in depression. Dr. Daniel Miller of Sunflower talks with Jill Daughhetee—Quality Improvement Advisor at Kansas Healthcare Collaborative—about the program and its early results.
Leaders in the Practice Transformation Network share success stories
|
|
|
The annual event's morning session included (back row, from right) Jenna Mikrut and Mallory Roberson from Community Health Center of Southeast Kansas, Dr. Daniel Miller from Sunflower Ob-Gyn, PA, and KHC's Devin June; and (front from right) Kelsey Moran, Bonnie Stephens, and Dr. Kim Allman from Family Physicians of Kansas, and Tiffany Trapp from Rush County Medical Clinic, and KHC's Jill Daughhetee. |
About 80 leaders across Kansas committed to clinical practice transformation and performance-based care came together last week near Salina for a full day of sharing knowledge and lessons learned at the 2018 Kansas PTN Annual Learning Event.
Among the featured speakers were seven local practice leaders who shared inspiring success stories of changing patient lives using evidence-based approaches for helping patients reduce their blood pressure. Their efforts were supported in part by a partnership between Kansas Healthcare Collaborative and the Kansas Department of Health and Environment.
One of the seven practices is Community Health Center of Southeast Kansas. Mallory Roberson — Population Health Manager who oversees the project at CHCSEK — said the clinic made substantial strides in building relationships with most of the patients who agreed to participate in the program, in addition to seeing improvements in health outcomes.
Winfield Pharmacy to host Blood Pressure Self-Monitoring Pilot Program

Winfield Pharmacy Health Mart was recently selected as one of only two communities to serve as a pilot for a YMCA Blood Pressure Self-Monitoring Program (BPSM). Grant-funded by the Kansas Department of Health & Environment (KDHE), this is a new partnership between KDHE and the YMCA.
Local clinic in Phillipsburg, Kansas is helping diabetic patients improve their health
More than half the diabetic patients of Phillips County Health Systems in Phillipsburg, Kansas participated in a program providing diabetic support and education.
In 2015, the first year of the program, 90 patients with chronic diabetic issues were referred to the Phillips County clinic. Of that number, 60 agreed to start the program. Nationally, on average just one-in-seven persons referred to diabetic programs are willing to participate.
Practice works to reduce labor intensive claims-based reporting
Using data to improve care plays an essential role in delivering quality healthcare for patients, and succeeding in the Merit-Based Incentive Payment System (MIPS). Barriers such as cost, limited staff, and convenience often restrict access to the tools necessary to track and send quality data to CMS. As a result, submitting quality data to MIPS through the CMS web interface, or a third-party data-submission service such as an EHR (Electronic Health Record) registry, or a qualified clinical data registry is not always an option for smaller practices. For those practices that fit this scenario, claims-based reporting is usually the only option. With claims-based reporting, clinicians must use codes specified by CMS that indicate a particular quality measure was performed with a patient. For healthcare professionals, the claims-based method can be difficult to track and labor intensive.
Satanta District Hospital testimonial
“My personal experience with KHC has been instrumental in changing the way we do things here. Through the camaraderie and sharing of ideas and information for making changes we have achieved a team that is always ready to rise to any challenge that is put before us.
Because we are a very small CAH, we need help with designing programs that impact patient care, family involvement and nurse and physician participation, we have found a wonderful resource in KHC. I have called or sent emails whenever we have something that we want to work on.
Coffeyville Regional Medical Center - Culture of Safety
Coffeyville Regional Medical Center - Culture of Safety
Click here to view the 2017 AHA Rural Conference Coffeyville Regional Medical Center’s storyboard video that highlights a Culture of Safety improvement project at their facility in Coffeyville, Kansas.
Click here to read more. (PDF)
Wesley Medical Center - Sepsis Case Study
Wesley Medical Center
HEN 2.0 Sepsis Case Study
Click here to view the video
Labette clinic is seeing a valuable exchange of information through PFAC
 The feedback goes both ways between the Patient and Family Advisory Committee (PFAC) and the Labette Health Physicians Group, according to Missy Beasley. Recently she was invited to present at the PFAC meetings at Labette Health in Parsons, Kansas.
The feedback goes both ways between the Patient and Family Advisory Committee (PFAC) and the Labette Health Physicians Group, according to Missy Beasley. Recently she was invited to present at the PFAC meetings at Labette Health in Parsons, Kansas.
Beasley is the clinic manager of the 25 physician and NPP multi-specialty clinics located in Parsons, St. Paul, Erie, Altamont, Cherryvale and Independence. Her clinic is a member of the Kansas Healthcare Collaborative Practice Transformation Network (PTN). It was one of the first to join, in October 2015. Beasley works with Josh Mosier, PTN Quality Improvement Advisor. Through their work on the PTN improvement measures, particularly patient involvement, Beasley said a PFAC committee was something the hospital-owned clinic had been wanting to set up. She was glad to join the hospital’s group which comprises 11 community patient and family advisors, one Board of Trustee liaison, and five or six hospital employees.
Finding a simple tool that results in many positive changes
Sumner County Family Care Center clinic partners
From Left: Lacie Gregory MD, Stephen Hawks DO, Joel Weigand MD, Steven Scheufler MD, Shana Jarmer MD, (not pictured Larry Anderson MD)
Amber Dawson hadn’t been at her new job as Administrator of Sumner County Care Center more than a few days when she ran across an email from Practice Transformation Network advisor Jill Daughhetee.
The Sumner County Care Center in Wellington has 11 providers and 30 employees and is celebrating 40 years of service this year. However, a recent string of turnovers in the administrator position had left the lines of communication down and employee morale down, too. Amber wanted to change that and Jill’s email offered some tools.
Together we're better
Frequently unintentional silos keep team members and co-workers from collaborative work. It happens in many organizations, including health care. People on different teams, who don’t see one another often or at all, may miss what ought to be obvious chances to work collaboratively.
With a new take on an old adage, making sure the right hand knows what the left hand is doing can make a big difference in providing better patient outcomes, more efficiency and cost savings.
Clinic finances move back into the black thanks to PTN participation
“It was incredible,” said Mary Barrett, office manager of her husband’s family practice in Neodesha, Kansas. After less than three months of work with the Kansas Practice Transition Network (PTN), she has made adjustments that “have been a game changer” in Dr. Bradley Barrett’s clinic.
Kansas PTN Quality Improvement Advisor Jill Daughhetee first met Mary in January and together they performed a Baseline Practice Assessment. “Jill analyzed our strengths and weakness,” Mary said, and candidly added, “we have some weaknesses.” With this list, they got started.
Preventive care getting a boost at the Eureka Clinic
Focus on the whole patient means special attention to preventive care.
This single practitioner clinic serves all of Greenwood County Kansas and beyond. Jennifer Larsen is the physician’s assistant. “We’ve tried to focus on whole patient care, especially preventive care,” she said.
“Secret Patients” provide feedback
Ottawa Family Physicians in Ottawa, Kansas have found an effective tool to get patient feedback. “It’s just very simple,” said Betty Franklin, administrative assistant.
Franklin explained that two or three weeks ahead of time, they look through the patient schedule and randomly pick three or four patients. A staff member calls them and asks if they would be willing to be a “secret patient.” If they agree, a Patient Satisfaction Survey is mailed to them, along with a self-addressed, stamped envelope.
Labette Health - Adverse Drug Events Case Study
Labette Health
HEN 2.0 Case Study: Adverse Drug Events
Click here to view the video