
Care transitions, particularly from an inpatient setting to home, can be a challenging time for patients who may be dealing with a medical crisis, a new medical condition, or change in care plan. Poor transitions of care can lead to a variety of negative outcomes, including medication discrepancies, adverse clinical events, poor patient experience of care, and frequently avoidable hospitalizations. Improving care transitions has been an important strategy for reducing the costs associated with hospitalization and readmissions1 and proves to be an important opportunity for addressing social determinants of health2. Transitional Care Management (TCM) serves to manage this hand-off period offering an excellent opportunity for primary care providers to oversee and coordinate support for a patient's medical conditions, mental health or behavioral health needs, social services, and other barriers to optimal patient outcomes.
Clay County Medical Center (CCMC) is a 25-bed Critical Access Hospital located in north-central Kansas with five Rural Health Clinics (RHCs) serving Clay Center and the surrounding counties. CCMC, a Compass HQIC hospital identified opportunities for improvement in their transitions of care, particularly between the hospital inpatient setting and their CCMC RHC clinics.
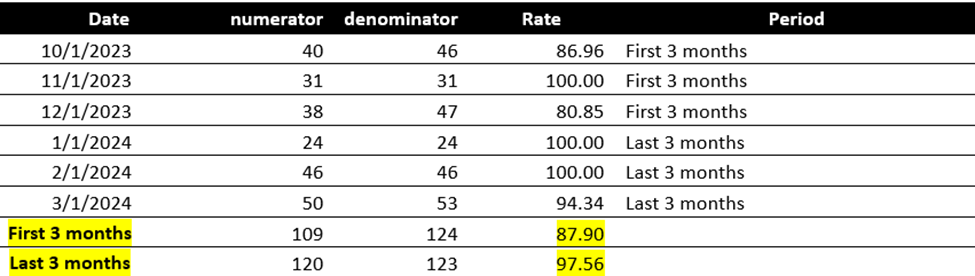
In October 2023, CCMC began a quality improvement project focused on increasing the rate of patients who are seen within seven days of hospital discharge through improving the transitions of care process after an admission to CCMC. In October 2023, at the beginning the project, 86.96% of CCMC patients were seen for post-discharge follow-up appointments within seven days from discharge. They set a lofty goal of achieving 100% of patients being seen for follow-up appointments within seven days after discharge from CCMC by March 2024.
The hospital observed that not all patients were remembering their follow up appointments or remembering to call and make an appointment after hospital discharge. They found that once home from discharge the patients didn’t always understand the discharge information that was given to them during the discharge process. CCMC also discovered that the information shared with primary care regarding the inpatient stay (specific needs such as medical interventions, medications, support needs, discussions concerning the need for a higher level of care, comfort care or end of life decisions, family dynamics, SDOH barriers, etc.) were not being communicated to the primary care team in the CCMC RHCs or may not have been occurring in a timely manner. In some cases, the primary care teams did not know where to access the missing information.
 |
||
| CCMC TCM Team, Pictured Above from Left: Jessica Badsky, Melissa Spellman, Jeanette Collin, Janet Fisher, Claudine Irwin, Trisha Finkbiner, and Julie Crimmins. Not pictured, Aspen Elledge. |
-
Be diligent about completing follow-up phone calls and the follow up appointments, ensuring that the patient is continuing to improve and if not, assisting in managing next steps.
-
Verify that the patient knows when their follow-up appointments are and that they have a plan to show up at the visit.
-
Confirm that the patient was able to pick up any new medications.
-
Establish that support services contact was made.
-
Elicit feedback about their stay while in the hospital and pass on compliments. Work towards improving areas that fell short of expectations.
- Educate, communicate, and follow up regularly with the RHC team shared RHC patients and work to improve transitions in care, patient quality of life and outcomes, decrease unnecessary readmissions, and foster teamwork.
The CCMC Transitional Care Management (TCM) program was designed using the Medicare billing requirements for TCM as a foundation. CCMC attempted to call all patients that returned home to the community within two business days to check on their status and to evaluate if there was a need for further support from CCMC or community-based services. Outreach was provided primarily by the CCMC social worker. The hospital provided training for the stakeholders, including the RHC team members, providers, board members, and executive team regarding the importance of effective care transitions and on how to use Cerner to view and share care transitions information. The team utilized a tracking system to provide a monthly review of care transitions for all key stake holders.
The work has not been without challenges. The team reports that even after workflows are implemented, it is easy for staff to fall back into old behavior patterns. Effecting permanent change is a work in progress. Billing TCM services remains a challenge. The setup process in Cerner required to lay the groundwork for billing has been complex. CCMC is currently collaborating with other Cerner facilities to review their documentation workflows and reimbursement though those collaborations are a challenge in itself as successful billing for TCM services is still not commonplace in rural Kansas communities, so opportunities to share information are limited. The team is still working to design workflows that best benefit the patient and the RHC.
 |
||
| Performance rates for CCMC for the Project Period October 2023 through March 2024 for the Post-Discharge Follow-Up Appt Measure. |
During the project period, CCMC’s performance increased from 86.96% in October 2023 to an average of 87.90% for the first three months and 97.56% for the last three months of the project. Despite the improvement, the project is still ongoing. CCMC has not yet reached their goal of 100% but still considers aiming for perfection their long-term goal.
Julie Crimmins, Director of Inpatient Services at CCMC says they will know they are successful “When we are able to share patient centric information consistently to provide for improved transitions in care, whether that be for a TCM or advance care planning visit, follow up care for chronic conditions, or continued preventative care maintenance.”
Julie reports that they have noticed other benefits to the TCM program. “It has helped us identify systems within the hospital that are working well and any areas that might need to improve. We get great feedback from the perspective of the patients and our internal customers. When the patient says there is a problem, listen,” advises Crimmins.
For example, through patient feedback, they identified that there was potential for improvement in medication reconciliation procedures in the organization. The clinic workflows for medication reconciliation were very different than in the hospital setting. These workflows are labor intensive. Before the project medication reconciliation was not a hard-wired process with a standardized step-by –step approach. After the first quality improvement project was completed in March 2024, the process has been established with a three-part approach including the aide, the nurse, and the medical provider. The goal is to manage and complete the medication history and reconciliation in the clinics timely and effectively.
Future planned quality improvement projects related to their efforts to improve transitions of care include increasing the percentage of patients who complete Advanced Care Planning and tracking and streamlining processes for medication reconciliation in the RHCs.
